Zyloprim
"Purchase zyloprim toronto, symptoms 5 days before missed period".
By: G. Kapotth, M.A., Ph.D.
Assistant Professor, University of Texas at Tyler
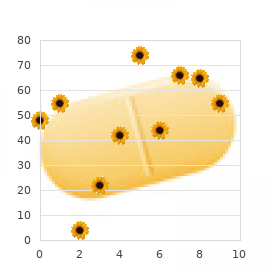
However symptoms 2 discount 100 mg zyloprim, in this situation the clinician would have to be very confident of their prediction [12] treatments yeast infections pregnant purchase zyloprim 100 mg free shipping. Many of the factors that predict a high early risk of death also predict a high risk of longterm dependency if the patient survives. Methods of prediction A variety of different approaches have been taken in predicting outcome after stroke. The singlefactor approach the simplest method is to identify a single factor, the presence or absence of which early after the stroke indicates the likelihood that the patient will have a good or bad outcome. The most widely used examples are age, severity of the neurological deficit, reduced level of consciousness, or lesion size, which have each been related to poor survival and functional outcome [12, 38]. Although such models are simple to use, and can guide clinical management, the user must be aware of their inaccuracy. Higher age, a severe neurological deficit, a reduced level of consciousness, and a large lesion size in the first few days after stroke are each associated, in general, with a poor outcome. Unfortunately, this association is not reliable enough to be anything other than a very rough guide to prognosis in managing individual patients. Nonetheless, such models have been used to stratify groups of patients by predicted prognosis in large randomized trials [42]. Indeed, large randomized trials provide an excellent opportunity to test such predictive models prospectively [43, 44]. Stroke scales the extent of brain damage In general, the greater the volume of brain damaged the worse the clinical outcome, except for critically sited strokes, particularly in the brainstem, where even quite small lesions can be fatal. Many of the clinical indicators of poor prognosis relate quite closely to the size of the brain lesion. For ischemic stroke, imaging generally adds little to the accuracy of clinical predictors [36]. This is not surprising, because the extent of the infarct on brain imaging can often be predicted from the clinical findings. In general, the larger the stroke lesion, the worse the likely outcome, except for small, critically sited lesions, which may be associated with a poor outcome. These provide scores which, depending on the presence, absence, or severity of various neurological impairments, are frequently used to describe the severity of stroke in the acute phase and have also been used to predict outcome. Predictions based on measures of function early after a stroke Scales such as the Barthel Index have been used to predict eventual functional outcome and may be particularly useful for those working in rehabilitation facilities [45, 46]. Predictions for individuals would then depend on the pattern of recovery observed in large cohorts of patients. Although these are generally more accurate than models based on a single variable, these are usually not sufficiently accurate to guide clinical decision making at the level of the individual patient, and many are limited by intrinsic methodological shortcomings and by an absence of external validation [12]. If such models are to be used in routine clinical practice, they need to be further refined, and then tested in large independ- the most common method of prediction is the informal judgments we make about patients during our daily work. The accuracy seems to be similar to those of mathematical models, at least in predicting a simple dichotomous outcome (dependent or independent), but this is bound to depend on the experience of the clinician [49]. In patients with acute stroke admitted in tertiary care centers, early prediction of a poor functional outcome or death by the treating physician was correct in about 90% of the cases [50, 51]. However, the ability to predict future quality of life was substantially less good [51]. In addition, a consequence of the increasing trend that clinicians specialize in certain phases of disease management. This is likely to limit their ability to predict functional outcome and quality of life correctly.
In fact medicine organizer box purchase 300 mg zyloprim with visa, the evidence available from randomized trials suggests that early supported discharge schemes are marginally cheaper overall than more prolonged hospitalbased rehabilitation (Section 19 medicine just for cough cheap zyloprim 100 mg otc. A practical approach to monitoring the cost effectiveness of a stroke service might include collecting data about the total length of stay in hospital. However, note would have to be taken of any major changes in nursing costs or those related to investigations and References 925 treatment. It is easy to reduce the length of stay by discharging patients into nursing homes instead of to their own homes, and by discharging more severely dependent patients into the community, but this adds to the costs (financial, physical, and emotional) to the family and social services. Except for billing purposes, setting up systems for collecting detailed data about exactly what investigations, drugs, and therapy patients receive would be timeconsuming and expensive, and would probably provide little extra information about the overall cost of care. An organized stroke service is likely to be cheaper than a disorganized one, and it could release resources for other areas. A comparison of the costs and survival of hospitaladmitted stroke patients across Europe. Immediate computed tomography scanning of acute stroke is costeffective and improves quality of life. Organisation of stroke care: education, referral, emergency management and imaging, stroke units and rehabilitation. Alternative strategies for stroke care: a prospective randomised controlled trial. Alternative strategies in stroke: randomised controlled trial of three strategies of stroke management and rehabilitation. Is the rapid assessment clinic rapid enough in assessing transient ischaemic attack and minor stroke Recent advances in managementof transient ischaemic attacks and minor ischaemic strokes. Use of tissuetype plasminogen actibator for acute ischemic stroke: the Cleveland area experience. Recommendations for comprehensive stroke centres: a consensus statement from the brain attach coalition (report). A systematic review and metaanalysis of randomized controlled trials of endovascular thrombectomy compared with best medical treatment for acute ischemic stroke. Populationbased study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. Triaging transient ischaemic attack and minor stroke patients using acute magnetic resonance imaging. The need for urgency in identification and treatment of symptomatic carotid stenosis is already established. Prevention of a first stroke: a review of guidelines and a multidisciplinary consensus statement from the National Stroke Association. Stroke: from recognition by the public to management by emergency medical services. The delay in reporting symptoms of carotid artery stenosis in an atrisk population. The Asymptomatic Carotid Atherosclerosis experience: a statement of concern regarding watchful waiting. Sustained benefit of a community and professional intervention to increase acute stroke therapy. Improving the efficiency of delivery of thrombolysis for acute stroke: a systematic review. Validity of indirect comparison for estimating efficacy of competing interventions: empirical evidence from published metaanalyses. Multicenter comparison of processes of care between stroke units and conventional care wards in Australia. Establishment of primary stroke centers: a survey of physician attitudes and hospital resources. Stroke care delivery in institutions participating in the Registry of the Canadian Stroke Network. A study of the workload and effectiveness of a comprehensive acute stroke service. Interactions within stroke systems of care: a policy statement from the American Heart Association/ American Stroke Association.
Lowdose and highdose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial medications related to the lymphatic system buy generic zyloprim 100mg line. Risk of primary intracerebral haemorrhage associated with aspirin and nonsteroidal antiinflammatory drugs: casecontrol study medicine river animal hospital buy zyloprim 100mg low cost. Risk of gastrointestinal haemorrhage with long term use of aspirin: meta analysis. Association between aspirin and upper gastrointestinal complications: systematic review of epidemiologic studies. Thrombotic thrombocytopenic purpura associated with ticlopidine in the setting of coronary artery stents and stroke prevention. A randomized comparison of clopidogrel and aspirin versus ticlopidine and aspirin after the placement of coronaryartery stents. Randomized comparison of ticlopidine and clopidogrel after intracoronary stent implantation in a broad patient population. Facilitation of sensory and motor recovery by thermal intervention for the hemiplegic upper limb in acute stroke patients: a singleblind randomized clinical trial. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention. Aspirin plus clopidogrel as secondary prevention after stroke or transient ischemic attack: a systematic review and metaanalysis. What is the role of dipyridamole in longterm secondary prevention after an ischemic stroke or transient ischemic attack Dipyridamole for preventing recurrent ischemic stroke and other vascular events: a metaanalysis of individual patient data from randomized controlled trials. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: timecourse analysis of randomized trials. Oral anticoagulants versus antiplatelet therapy for preventing further vascular events after transient ischaemic attack or minor stroke of presumed arterial origin. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. A randomized trial of anticoagulants versus aspirin after cerebral ischemia of presumed arterial origin. Major bleeding during anticoagulation after cerebral ischemia: patterns and risk factors. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Atrial fibrillation and thromboembolism: a decade of progress in stroke prevention. Oral anticoagulants for preventing stroke in patients with nonvalvular atrial fibrillation and no previous history of stroke or transient ischemic attacks. Are the results of randomized controlled trials on anticoagulation in patients with atrial fibrillation generalizable to clinical practice Translating the results of randomized trials into clinical practice: the challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Optimal oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and recent cerebral ischemia. An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation. Increased risk of intracranial hemorrhage when aspirin is combined with warfarin: a metaanalysis and hypothesis. A clinical trial comparing three antithromboticdrug regimens after coronaryartery stenting. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an openlabel, randomised, controlled trial. Edoxaban versus References 853 286 287 288 289 290 291 292 293 294 295 296 297 298 warfarin in patients with atrial fibrillation. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta analysis of randomised trials.
Careful periodic evaluation of the optic nerve and visual field testing are essential in the management of glaucoma treatment innovations buy genuine zyloprim online. Stereophotographic documentation of the optic nerve or computerized imaging of the optic nerve or retinal nerve fiber layer aids the detection of subtle changes over time internal medicine order zyloprim toronto. Visual field loss should correlate with the appearance of the optic nerve; significant discrepancies between the pattern of visual field loss and optic nerve appearance warrant additional investigation, as noted in Chapter 3. Fluctuation of intraocular pressure and glaucoma progression in the early manifest glaucoma trial. Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer, and Tono-Pen. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Older age the Baltimore Eye Survey found that the prevalence of glaucoma increases dramatically with age, particularly among individuals of African descent, whose prevalence exceeded 11% in those older than 80 years. Therefore, older age appears to be an independent risk factor for the development and progression of glaucoma. In addition, glaucoma is more likely to be diagnosed in black patients at a younger age and at a more advanced stage than it is in white patients. As mentioned previously, black patients have thinner corneas on average than white patients. Evaluation of the optic nerve head is particularly challenging in highly myopic eyes that have tilted discs or posterior staphylomas. Also, the myopic refractive error may cause minification of the optic nerve, further complicating accurate optic nerve assessment. Myopia-related retinal degeneration or anomalies can cause visual field abnormalities that are difficult to distinguish from those caused by glaucoma. In addition, patients who are highly myopic may have difficulty performing accurately on visual field tests, making interpretation of visual field abnormalities more challenging. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Associated Disorders Diabetes mellitus There is controversy as to whether diabetes mellitus is a risk factor for glaucoma. However, the Framingham Study, the Baltimore Eye Survey, the Barbados Eye Study, and a revised analysis of the Rotterdam Study did not find a significant association. Furthermore, the Rotterdam Study and the Barbados Eye Study, which were large longitudinal population-based studies, did not identify diabetes as a risk factor for the development of glaucoma. However, the cohort of diabetic patients was skewed, because the presence of retinopathy was an exclusion criterion for this study. Hypertension the Baltimore Eye Survey found that systemic hypertension was associated with a lower risk of glaucoma in younger (<65 years) subjects and a higher risk of glaucoma in older subjects. The hypothesis is that younger individuals with high blood pressure may have better perfusion of the optic nerve, but as these patients age, their chronic hypertension may have adverse effects on the microcirculation of the optic nerve and increase its susceptibility to glaucomatous optic neuropathy. Conversely, in the Barbados Eye Study, the relative risk of developing glaucoma among subjects with systemic hypertension was less than 1. The overtreatment of systemic hypertension may contribute to glaucoma progression in some cases (eg, normal-tension glaucoma) and should be monitored. Other associated conditions Sleep apnea, thyroid disorders, hypercholesterolemia, migraine headaches, low cerebrospinal fluid pressure, corneal hysteresis, and Raynaud phenomenon have variously been identified in some studies as potential risk factors for the development of glaucoma. The patients at greatest risk of blindness are those who present with visual field loss at the time of diagnosis. For patients with decreased visual function, a referral to a vision rehabilitation specialist should be considered. These specialists can help improve visual function by optimizing lighting, enhancing contrast, reducing glare, and providing adaptations to enhance activities of daily living.
If a reaction is suspected treatment medical abbreviation generic zyloprim 100 mg with visa, an ocular hypotensive agent with an alternative preservative or preservative-free formulation can be used (see Table 7-2) medicine 1800s purchase line zyloprim. For rehabilitation of the ocular surface, it may be beneficial to stop all topical medications-if the level of glaucomatous damage permits-and have the patient use preservative-free artificial tears frequently. Patients sometimes fail to associate systemic adverse effects with topical drugs and, consequently, seldom volunteer symptoms. In addition, communicating with the primary care physician is important not only to provide information about the potential adverse effects of glaucoma medication but also to discuss the effects that other currently prescribed medications (eg, for systemic disease) might have on the glaucomatous process. Administration of Ocular Medications Patients should be shown how to instill eyedrops properly and should be given instruction on nasolacrimal occlusion, which can be used to reduce the systemic absorption of topical ocular medications and to prolong their ocular contact time. Patients should be taught how to space their medications, and instructional charts should be given. A dosing aid device may also be considered, especially for patients who live alone or who are unable to successfully instill eyedrops. However, glaucoma patients who are pregnant frequently continue to require ocular hypotensive medical therapy throughout the pregnancy. As mentioned previously, topical ocular hypotensive medications are systemically absorbed; they subsequently cross the placenta and enter the fetal circulation or can be secreted into breast milk. Unfortunately, there is little definitive information concerning the safety of glaucoma medication use in pregnant women or breastfeeding mothers. The Pregnancy Category C rating indicates that no animal studies have been conducted and that it is not known whether the drug can cause harm when given to a pregnant woman. This category also includes drugs that have shown an adverse effect in animal studies, but there are no adequate and well-controlled studies of these drugs in pregnant women. Brimonidine is the only glaucoma agent with a Pregnancy Category B rating; all other agents have a Pregnancy Category C rating. There are reports of growth retardation, arrhythmia, bradycardia, and lethargy affecting the fetus or newborn exposed to b-adrenergic antagonists. These agents are concentrated in breast milk and should be avoided in breastfeeding mothers because of their potential adverse effects on infants. If a b-adrenergic antagonist must be used during pregnancy or during breastfeeding, the fetus or infant must be carefully monitored and the lowest effective dose should be utilized. Brimonidine, though reasonably safe to use during pregnancy, has been reported to cause apnea in infants and young children and should not be used in these patients. Brimonidine should be discontinued prior to delivery to minimize the risk of this complication in the newborn. Because prostaglandins increase uterine contractility and may induce labor, albeit when given at much higher doses than those used in topical therapy, there is a theoretical risk to the pregnancy. With all topical ocular hypotensive medications, pregnant and breastfeeding patients should be advised to perform nasolacrimal occlusion during eyedrop instillation. In general, it is prudent to minimize the use of medications in pregnant women whenever possible. The clinician may want to consider laser trabeculoplasty or other surgical intervention in cases in which the benefits outweigh the potential risks. Use of Glaucoma Medications in Elderly Patients There are specific considerations regarding the use of glaucoma medications in elderly patients. First, elderly patients generally have greater difficulty instilling their medications than do younger patients; consequently, their adherence to the treatment regimen may be affected. Instillation difficulties may be due to tremor, poor coordination, or a comorbidity such as arthritis. Adherence will also be affected in an elderly patient with reduced mental capacity or poor memory and a complicated drug regimen, especially because this individual is most likely already taking multiple systemic medications for other ailments. Second, elderly persons have a greater susceptibility to the systemic adverse effects of glaucoma medications. The incidence and severity of systemic adverse effects may be higher with b-blockers and a2-adrenergic agonists in these patients. For example, it has been shown that a significant proportion of asymptomatic elderly patients suffer a significant, but reversible, reduction in pulmonary function with the use of b-blockers. Avoiding unsuspected respiratory side-effects of topical timolol with cardioselective or sympathomimetic agents. The use of lower-cost generic medications has been shown to improve patient adherence to medication regimens.