Cymbalta
"Buy 60mg cymbalta fast delivery, anxiety symptoms 8-10".
By: G. Thorus, M.A.S., M.D.
Assistant Professor, Nova Southeastern University Dr. Kiran C. Patel College of Osteopathic Medicine
Encourage your teen to contact campus services to request accommodations anxiety 30 minute therapy 60mg cymbalta visa, if needed anxiety symptoms - urgency and frequent urination order generic cymbalta from india, if he/she will be attending college. Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Transition and transfer from pediatric to adult care of young adults with complex congenital heart disease. In addition to identifying a medical home, the adolescent and young adult patient should receive education and a plan about where to seek care in certain situations (4,7). Without a clear plan, patients are often confused about whom to call or where to seek treatment in the case of medical problems. While a plan can be established for the medical home provider to serve as the medical gatekeeper, it is often better to give the patient specific guidance for certain situations. Psychological Issues Adolescents and young adults with chronic disease are often transferred to an adult provider, not at a certain age or level of maturity, but when they begin to display "adult" behaviors. These behaviors can include pregnancy, substance abuse, criminal activity, and noncompliance (16,25). This signifies the level of psychosocial issues that exist in this population and the importance that it must play in a transition program. Biopsychosocial experiences of adults with congenital heart disease: review of the literature. Basic screening for psychosocial disorders must be a part of the transition process. While these numbers are no different than age-matched controls, it illustrates the prevalence of these behaviors in an already at-risk population. Transition programs should stress education regarding the harmful effects of substance abuse and other high-risk behaviors (31). Therefore, any patient at an elevated risk for a sudden and life-changing medical event should be encouraged to complete an advance directive (4,7,9). In most instances, this discussion should occur with the pediatric provider prior to the transfer of care (7,33). This allows the process to be a gradual introduction to the idea of advance directives and allows the patient and their family to be adequately prepared to make these difficult decisions. Also, it allows the concept to be introduced and the discussion started by a provider that has an established relationship with the patient and their family. Noncardiac Medical Care Routine medical issues that can be handled by the primary care provider are the health maintenance issues like smoking cessation, weight loss/management, hypertension/lipid screening, oral care, and substance abuse counseling. These include erythrocytosis, cholelithiasis, abnormal hemostasis, renal dysfunction, hyperuricemia, hypertrophic osteoarthopathy, and scoliosis. Reproductive Health A vital part of the transition process involves education regarding reproductive health issues. This information should include genetic counseling as well as how their own comorbidities and life expectancy may weigh into their family planning decisions. For female patients, education on reproductive health should be much more involved to include discussions regarding contraception and pregnancy (4,7,9,37) (see Chapter 69). Employment, Insurance, Disability, and Government Aid the importance of employment and insurance cannot be understated. Structured career counseling and employment advice has been shown to be associated with a higher rate of employment (73%) compared to those who received no counseling or advice (46%) (40). Discrimination in the workplace is unlawful and three main legislative acts protect patients with disabilities: 1. This prohibits employment discrimination based on disability by any federal employer programs that receive federal funding (41). This allows the progression of disability to be paid by a special second-injury fund to ensure that employers are protected from future losses.
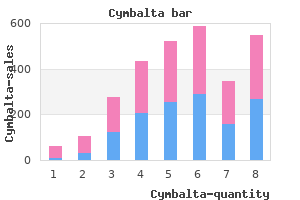
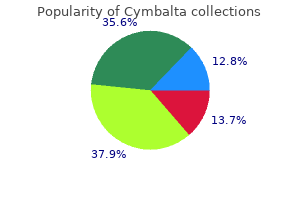
Pulmonary artery hypertension and small birth weight for gestational age were associated with worse survival rates anxiety hot flashes purchase cymbalta 20mg on line. This includes an extensive evaluation for chronic reflux and aspiration anxiety symptoms 3 weeks cymbalta 30 mg lowest price, structural airway abnormalities (such as tonsillar and adenoidal hypertrophy, vocal cord paralysis, subglottic stenosis, and tracheomalacia), and assessments of bronchoreactivity (352). Management of children with pulmonary vein stenosis is difficult as catheter-based interventions or surgery have shown poor long-term results and overall survival is poor with the 2-year survival rate from diagnosis of 43% (338). Treatment with afterload reduction and diuretics may show benefit in this select group (359). However, the condition can occur rarely, and an accurate diagnosis is essential for treatment (26,363,364). Predisposing factors include an indwelling central line, collagen vascular diseases, thrombophilia, bacterial endocarditis, and ventriculoatrial shunt for the treatment of hydrocephalus. Likewise, the use of oral contraceptive agents may cause hypercoagulability, leading to pulmonary thromboembolic phenomena. Therapy in adults is evidence based whereas in children it is frequently based on experience. Numbers above the bars indicate the percentage of patients with pulmonary hypertension. The three major pathways (endothelin-1, nitric oxide, and prostacyclin) involved in the regulation of pulmonary vasomotor tone are shown. Endothelial dysfunction results in decreased production of endogenous vasodilatory mediators (nitric oxide and prostacyclin) and the upregulation of endothelin-1, which promotes vasoconstriction and smooth muscle cell proliferation. Advances in therapeutic interventions for patients with pulmonary arterial hypertension. Genetic testing is indicated for risk stratification (Class I; Level of Evidence B). Antibiotic prophylaxis for the prevention of subacute bacterial endocarditis in cyanotic patients and those with indwelling central lines (Class I; Level of Evidence C). The number in each group (brackets) and the predicted survival out of a possible 5 years is depicted. A positive response is defined by assessing the change hemodynamic parameters to vasodilators. The younger the child at the time of testing, the greater the likelihood of acute pulmonary vasodilation in response to vasoreactivity testing (155,367,368). Many oral and inhaled vasodilators have been used for testing vasodilator responsiveness (202,216,367,368,369,370,371,372,373,374,375). Digoxin is used in the presence of right ventricular failure, although there are no clear-cut data regarding its effectiveness in children (376). Diuretics are used to treat peripheral edema or ascites in the presence of right heart failure, however, excessive diuresis should be avoided. Careful attention to respiratory tract infections is required as they may worsen alveolar hypoxia, and routine influenza vaccination is recommended. However, oxygen therapy is not used as a mainstay of therapy in children with normal daytime saturations. Although the use of chronic anticoagulation has not been studied widely in children, it is usually recommended. The use of anticoagulation in patients with Eisenmenger syndrome is controversial and the potential risks and benefits of anticoagulation in this setting must be carefully weighed (246). Vasoreactivity Testing As in adults, cardiac catheterization with acute vasodilator testing is essential prior to selecting targeted therapy in children. Cardiac catheterization carries a greater risk in those children with baseline suprasystemic pulmonary arterial pressure (odds ratio = 8. Because adults treated with calcium channel blockers began to fail this therapy, Sitbon established more stringent criteria for defining acute vasoreactivity in adults. Although the more strict criteria are used in children, this has not been adequately studied in this population. In both children and adults without post-tricuspid valve shunts, acute vasoreactivity is associated with improved survival independent of the used criteria (32,156,384). Calcium Channel Blockers the use of calcium channel antagonists to evaluate vasoreactivity is dangerous, as these drugs can cause a decrease in cardiac output or a marked drop in systemic blood pressure (363).
The duration of anti-inflammatory treatment for rheumatic arthritis can usually be guided by symptoms and response to therapy anxiety symptoms in 12 year old boy buy cymbalta 30mg without prescription. In cases with severe symptoms anxiety symptoms and causes cymbalta 60mg overnight delivery, reported treatments include phenobarbital, haloperidol, valproic acid, corticosteroids, plasma exchange, and intravenous immune globulin (314,315,316,317,318,319). Although some of the older literature suggests a role for digoxin (56,300,320), this may have been due to the belief that myocardial dysfunction played an important role in rheumatic carditis. Our current understanding of the pathophysiology of rheumatic carditis suggests that digoxin is unlikely to be of benefit with the exception of rate control for cases with atrial flutter/fibrillation. It should be emphasized that the primary hemodynamic abnormality is valvular incompetence rather than myocardial dysfunction. Diuretics and afterload reduction may be valuable as temporizing measures in patients with significant regurgitation and symptoms. However, in cases with intractable heart failure, surgical restoration of valvular competency (repair or replacement) may be lifesaving (213,321). In particular, patients with a flail mitral valve after chordal rupture do not respond to medical management and require surgery (211,249) (see Table 59. In the absence of data on the natural history and impact of treatment on chronic valvular disease in children, many practitioners extrapolate from the adult literature and P. Asymptomatic patients with rheumatic valvular disease can often be followed conservatively as most remain stable for years. Anticoagulation with warfarin is recommended for patients with mitral stenosis who have a history of a prior embolic event, for those in atrial fibrillation, or for patients with a left atrial thrombus (27,241). In addition, some recommend anticoagulation for patients with severe mitral stenosis in sinus rhythm in the setting of marked left atrial enlargement (27,323). For those receiving warfarin anticoagulation, monitoring may be challenging in some settings, but is nonetheless critically important in preventing complications (27). Heart rate control may be beneficial for those with atrial fibrillation and a fast ventricular response (241). The role of afterload reduction in the management of asymptomatic patients with chronic severe mitral regurgitation and preserved left ventricular function remains unclear. Although some studies have demonstrated improvement in hemodynamic variables (324,325,326), other studies have suggested that vasodilators might result in hemodynamic worsening (327,328). At present, there are no long-term studies showing afterload reduction in this setting to delay the onset of symptoms, ventricular dysfunction, or improve outcome. Thus, use of afterload reduction in the management of asymptomatic patients with chronic mitral regurgitation who have preserved left ventricular function is not recommended (241,329,330). Once symptoms develop, medical management of mitral or aortic regurgitation has little role except as a temporizing measure, and surgical intervention is indicated (241). For patients with severe aortic regurgitation, hypertension should be treated, preferably with a dihydropyridine calcium channel blocker or angiotensin-converting enzyme inhibitor/aldosterone-receptor blocker. Medical therapy with angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers and beta blockers may be used in symptomatic patients with severe aortic regurgitation who are not candidates for surgery (comorbidities) (241). Retrospective studies have suggested that statins may slow the progression of both rheumatic mitral and aortic stenosis. The mechanism remains unclear; the anti-inflammatory properties of statins may play a role. Results from prospective trials in adults with valvar aortic stenosis have yielded conflicting results. Unless surgery is contraindicated for other reasons, such patients should be referred for surgery (241,322). Patients with rheumatic mitral stenosis and mild symptoms such as dyspnea on exertion related to higher heart rates may benefit from negative chronotropic agents, such as beta blockers or calcium channel blockers. Judicious use of diuretics and/or sodium restriction may be valuable in cases with pulmonary venous congestion (336). With significant stenosis and symptoms, both percutaneous balloon valvuloplasty (337,338) and surgical intervention have been effective (241,339). In patients with juvenile rheumatic mitral stenosis (age 20 years), balloon mitral valvotomy is not only safe and effective, but may provide better immediate results compared to adults (267). An echocardiographically determined mitral valve morphology score combining assessment of leaflet mobility, subvalvular thickening, leaflet thickening, and leaflet calcification has been found to be a predictor of outcome after balloon valvuloplasty for mitral stenosis (271,273,340).
Laser energy applied to the tip of a small wire has allowed controlled perforation of the atretic valve tissue and has been achieved in several patients with good results in short-term follow-up (80); however anxiety 1-10 rating scale buy generic cymbalta 20mg on line, laser therapy carries the disadvantages of increased risk to staff anxiety symptoms for no reason order cymbalta 40mg with amex, the requirement for protective goggles, limited portability, and considerable capital expense in the setting of an uncommon defect. Radiofrequency energy, which safely can achieve well-defined lesions of coagulation necrosis, is now widely applied in the treatment of many cardiac dysrhythmias. Radiofrequency wires capable of confining the energy to the tip have been developed for this lesion based on proven utility in recanalization of arterial occlusions and results have been encouraging. Where radiofrequency or laser wires have not been available, other means of attaining perforation have been used, including mechanical wire perforation and standard electrode catheters. The reported literature attests to the fact that it is possible to establish continuity from right ventricle to the pulmonary artery in the catheter laboratory and thus avoid the need for cardiopulmonary bypass in many patients (23,40,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102). A relatively recent analysis of patients undergoing initial transcatheter perforation of the pulmonary valve with an initial medial tricuspid Z-score of -5. Subsequent or concurrent stenting of the arterial duct may shorten the initial hospitalization and avoid the complications of prolonged infusions of prostaglandin analogous to the surgical strategy of undertaking a patch of the right ventricular outflow tract and concurrent shunt (103,104). In evaluating the literature one must be careful to distinguish an absolute increase in the size of an anatomic structure such as the tricuspid valve from that of the indexed size. As an example the tricuspid valve may appear to enlarge over time with transcatheter perforation of the pulmonary valve (105), however, the indexed Z-value may not appear to change significantly (23). In addition, the need for prolonged prostaglandin infusion, creation of a systemic-to-pulmonary artery shunt, or implantation of a stent in the ductus arteriosus to achieve the same end is a common occurrence in this group of patients and occurs in 33% to 58%. To further frustrate clinicians the timing of secondary intervention to increase pulmonary flow can be difficult to assess after transcatheter valvotomy as it appears that days to weeks are required for the decompressed right ventricular compliance to improve. If a systemic-to-pulmonary arterial shunt is created too early one can be in the paradoxical situation of occluding the same shunt in the future once the ventricular compliance has improved. To further complicate matters a systemic shunt in the setting of severe pulmonary insufficiency and tricuspid insufficiency can result in an ineffective "circular" circulation where flow of systemic arterial blood courses through the shunt to the right ventricle, regurgitates through the tricuspid valve to the right atrium, and courses across the atrial septum to the left atrium where the process repeats. Effective pulmonary flow is decreased and the left ventricle is exposed to conditions similar to a large arteriovenous fistula. Myocardial oxygen demand is increased, diastolic aortic pressure is borderline and the patient is cyanotic; all of which contribute to progressively worsening myocardial performance. Still consideration may be given to stenting the ductus concurrent with valve perforation in selected cases (104). It seems that the best outcomes are clearly achieved with an individualized cooperative creative transcatheter surgical approach including the so-called hybrid interventions (106,107,108,109). The role of transcatheter techniques in the management of these patients is in evolution, however, in at least one series it compared favorably to surgical outflow tract reconstruction (81). It is important to recognize that the postintervention period is characterized by a changing physiology that may include adjustment to postnatal life, right-to-left shunting at the atrial level, systolic myocardial dysfunction, potentially ineffective circulatory flow, restrictive right ventricular physiology, pulmonary stenosis and insufficiency and tricuspid insufficiency represents a tremendous challenge to postintervention management with few, if any, cardiac conditions being more complex to the intensive care unit. One cannot underestimate the influence of expertise in managing this challenging state when evaluating the influence of experience on outcome. With a relatively small number of patients affected by this condition, there is much to be learned from a multicentered approach to collecting a longitudinal experience in a combined transcatheter and surgical approach to a challenging clinical problem. Whereas a percutaneous approach may avoid or delay the use of cardiopulmonary bypass in the newborn period, it remains to be seen whether it results in a decrease of long-term morbidity or mortality. Treatment of the Adult It should be clear from the preceding discussions that there is great anatomic and physiologic diversity of patients surviving to adulthood with pulmonary atresia and intact ventricular septum. Patients may have achieved a biventricular circulation, a univentricular circulation in the form of a total cavopulmonary circulation or a permanently palliated shunted state. Outcome data for the adult population are few and reported results may even be counter intuitive. For instance, it is unclear whether a biventricular circulation holds advantage over a univentricular circulation in the assessment of exercise capacity and indeed may be more influenced by pulmonary than cardiac issues, as aerobic capacity appears decreased in both groups (70,110). Further, restrictive physiology associated with right ventricular pathology appears to play an important role (69). Myocardial perfusion abnormalities persist well beyond definitive repair (palliation) (111). In the adult with a biventricular repair right ventricular restriction may favor better physiologic status, although many patients will go on to require a pulmonary valve replacement to restore competency of the right ventricular outflow tract (69,112). In a recent study (113) of 20 survivors into adulthood (19 to 39 years old) with Fontan (n = 7), biventricular (n = 8), and palliated shunts (n = 5) there were five deaths at a mean of 32 years old. Atrial arrhythmias occurred frequently (80%) but ventricular arrhythmias were not uncommon (15%).