Dutas
"Generic dutas 0.5 mg with visa, hair loss curezone".
By: M. Curtis, M.B. B.CH. B.A.O., Ph.D.
Associate Professor, Washington State University Elson S. Floyd College of Medicine
Data for efficacy of Musculoskeletal Causes Trigger points on the anterior abdominal wall hair loss 6 months after chemo generic dutas 0.5mg online, in the vagina hair loss cure earth clinic order dutas 0.5 mg without prescription, or in pelvic floor may be amenable to injections of local anesthetic. If local anesthetic injection relieves pain, a series of injections with anesthetic and corticosteroids may provide long-term relief. Observational data have revealed that targeted injections are effective in 68% of patients with trigger point pain. It is estimated that 75% of women with suspected gynecologic etiologies of pain will have improvement of pain at one year postoperatively. It can involve resecting only the painful area of the vestibule, excision of the entire vestibule including skin, mucosa, and vestibular glands, or perineoplasty in which all tissue of the perineum just anterior to the anal sphincter is resected that may denervate the vestibule. In studies performed, success has been defined variably and complications are often not reported that makes results difficult to interpret. These modalities can promote collagen remodeling while destroying nerves and blood vessels that are abnormal in women with vulvodynia. Patients with severe, refractory disease can be offered cystoplasty or urinary diversion with or without cystectomy. However, pain can persist even after removal of the bladder, and pain in the diversion pouch has also been reported. Patient selection and counseling are crucial for these major surgeries, and providers experienced with these procedures in this patient population should be sought. For areas of point tenderness, trigger point injections of anesthetic solution with or without steroids can be administered. However, the patient must be cautioned that surgical scar revision like any surgery can lead to further scar formation, and it is not predictable as to whether the pain will recur. If there is concern for abdominal wall hernia as a cause of pain, the patient should be referred for appropriate testing and surgical treatment. This treatment has been assessed in primary and secondary dysmenorrhea and is effective at alleviating midline menstrual pain. Likewise, adhesiolysis is unlikely to provide long-term relief because this scar tissue can re-form. Neuromodulators implanted at higher levels can be used and are implanted by a neurosurgeon. Limited data have shown symptom improvement of 30% to 56% for up to three months, declining after that. Symptom improvement is reported to be long lasting (one to two years) at rates of 70% to 100%. In addition, there is some concern that laser treatment can lead to delayed bowel injury and perforation. Flares may require specific treatment in addition to what is done to manage pain on a regular basis. The nature of the pain can change as can other related symptoms and their impact on function. Providers must resist giving the patient a diagnosis or label that restricts treatment options. Prevalence and incidence of chronic pelvic pain in primary care: evidence from a national general practice database. Summary of the National Institute of Arthritis, Diabetes, Digestive and Kidney Diseases Workshop on interstitial cystitis, National Institutes of Health, Bethesda, Maryland, August 28-29, 1987. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. Do the National Institute of Diabetes and Digestive and Kidney Diseases cystoscopic criteria associate with other clinical and objective features of interstitial cystitis Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. Prevalence of interstitial cystitis/painful bladder syndrome in the United States. Modulation of pain and hyperalgesia from the urinary tract by algogenic conditions of the reproductive organs in women. The relationship between interstitial cystitis and endometriosis in patients with chronic pelvic pain.
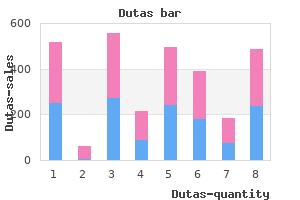
First hair loss in men over 65 purchase genuine dutas on line, as discussed above hair loss cure dec 2013 discount 0.5mg dutas amex, medical specialty boards credential individuals who complete standardized training, meet stated criteria, and pass examinations. In the second instance, credentialing is typically a locally driven process, subject to the constraints of institutions and the requirements of licensing bodies. Its goal is to ensure that the provider possesses the relevant knowledge, skills, and attitude to perform his or her duties within the set parameters of a chosen specialty or subspecialty. In other words, can a provider provide safe and high-quality patient care and work effectively in a team environment This is a key component of medical professionalism and, as such, is usually peer driven. While the process appears daunting, it is necessary to protect all parties involved including the applicant, the department, the hospital, and most importantly the patient. Predetermined standards and core skills established through common legal, professional, and administrative practices, endorsed by a formal consensus process, that are publicly available ensure the continued provision of optimal health care and hopefully produce an applicant who not only possesses all the attributes required to provide good medical practice but also shows a fitness to practice including clinical and educational competency, and establishment and maintenance of effective relationships with patients, acts with probity, and makes the care of the patient his or her first concern. There, with clear and standard departmental policies and procedures that the applicant must meet, there is typically a collection and authentication of all documentation supplied by the applicant. Within that, there is an assumption of area of medicine and demonstrate special knowledge and competencies in that field. Evidence must be presented that the new board will establish defined standards for training and that there is a system for evaluation of educational program quality. With this approval, the parent boards were given permission to set requirements and to develop the process for individual physicians to be certified as female pelvic medicine and reconstructive surgeons. Typically, such material includes proof of education and training, license, certification, experience, medical malpractice or negative clinical outcomes, and character references. Once credentialing has taken place, an applicant may be appointed on a probationary period ranging from 3 to 12 months enabling employers to observe the practical skills, clinical judgment, bedside manner, and collegial interaction of the applicant. Self-critique and review is crucial to the process, just as it is to the review of the applicant. During the reappraisal period, the applicant may request additional training or experience in new technology for privileges beyond the basic predetermined criteria such as what has occurred with the introduction of robotic surgery. If an applicant has dropped all or a portion of his or her practice and would like to reenter full-time practice, the credentialing division of a medical affairs department or a departmental chair needs to consider which pathway would best serve the applicant and the department; reentry may require formal reeducation, retraining, supervised experience, or simulation center training. Routinely, a departmental chair determines the criteria for clinical privileges and is satisfied that the applicant possesses the necessary experience to meet these criteria. Privileges are data driven and are based on demonstrated competence as reported by peer review. Peer review decisions must be fair, performed in good faith, not unreasonable, capricious, or arbitrary, have dated detailed documentation, and be justifiable and equally applied to all without bias. There must be no financial obligation to the proctor from the surgeon or the patient. Industrysupported proctors should be cleared through a hospital credentials committee and highly vetted and regulated. Ultimately, the Governing Board of the hospital makes the final decision based on the recommendations of the departmental chair and medical executive committee. Credentialing can be thought of as the minimum requirements that allow a provider to work in a health care setting, while privileging goes beyond that to determine what procedures are appropriate for particular providers to perform or, in other words, to determine in which procedures the surgeon has competency. Surgical competency (Table 26-2) is not based on surgical skill alone, but includes complete management and longitudinal care of the patient. In many institutions, privileging advanced surgical procedures is based on subspecialty certification. For example, privileges for performing a radical hysterectomy are only granted to a gynecologic oncologist at most institutions. This will be at the local level and may differ across geographic regions and between institutions depending on local customs and standards. At the same time, coming from a long-standing tradition and founding as pelvic surgeons, there are many ethical issues constant to any surgical field. One of the most significant ethical issues involves the incorporation of new treatments into clinical practice. In being true to the commitment of professionalism, as has been discussed in the sections "Credentialing" and "Privileging," in the face of the challenge of technology, we would be well served to appeal to those tools that are already in place, such as informed consent. The discussion of benefits, risks, complications, and alternative therapies is predicated on known "standards" for comparisons and options.
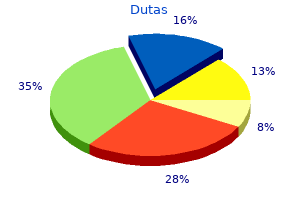
A 3D finite element model of anterior vaginal wall support to evaluate mechanisms underlying cystocele formation hair loss 9 months after baby order 0.5mg dutas overnight delivery. Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis hair loss cure close purchase dutas without prescription. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. The use of intraoperative cystoscopy in major vaginal and urogynecologic surgeries. The incidence of ureteral obstruction and the value of intraoperative cystoscopy during vaginal surgery for pelvic organ prolapse. Anatomic relationships of the distal third of the pelvic ureter, trigone, and urethra in unembalmed female cadavers. Little is known about the underlying mechanisms that cause pelvic floor dysfunction. Historically, theories regarding the pathophysiology of pelvic floor disorders have been derived from observation of success-or failure-of new surgical or medical therapies. Therefore, our understanding of the possible mechanisms behind pelvic floor disorders continues to evolve. In this articler, mechanisms of pelvic floor dysfunction will be reviewed to address hypothesized theories of the pathophysiology of urinary and anal incontinence, overactive bladder, and pelvic organ prolapse. However, the bead chain cystourethrogram was ultimately found to be poorly reproducible and was eventually abandoned. The concept of pressure transmission is important with respect to mechanisms of urinary incontinence. Specifically, continence is maintained during increased intra-abdominal pressure if the pressure in the urethra exceeds the pressure in the bladder. The absolute difference between urethral pressure and bladder pressure is described as the "closure pressure," typically measured during urodynamic testing. If the closure pressure drops below zero (eg, if bladder pressure exceeds urethral pressure), incontinence will occur. In women with stress incontinence, the closure pressure decreases to zero (or below zero) during increased intra-abdominal pressure. A metallic bead chain has been inserted transurethrally and lateral radiography demonstrates the angle formed by the posterior urethra and bladder base. Furthermore, if the urethra descends through the levator hiatus at the instant of increased intra-abdominal pressure, the urethra will not be exposed to the increase in intra-abdominal pressure. This may result in an unfavorable pressure gradient between the bladder and urethra, resulting in incontinence. For almost four decades, hypermobility of the urethra has been defined by the "Q-tip test" or cotton swab test. A positive cotton swab test is defined as rotation beyond 30% from the horizontal during straining. Weakness of the muscular component of the pelvic floor contributes to hypermobility. Reduction in coaptation or in the striated or smooth muscle tone can leave the urethra open at rest, facilitating stress incontinence. A transient reduction in urethral tone may be associated with -adrenergic antagonists. Mostly, overactive bladder is thought to be a result of involuntary detrusor contractions. However, in childhood, acquisition of bladder control is achieved through cortical maturation, with the inhibition of involuntary detrusor activity. Children who fail to acquire this suppression of detrusor activity may be prone to nocturnal enuresis or other manifestations of overactive bladder. The urodynamic catheter is drawn through the urethra, resulting in a display of urethral pressure from proximal to distal. In each panel, the tracing, from top to bottom, represents bladder pressure, abdominal pressure, calculated detrusor pressure, urethral pressure, and calculated urethral closure pressure. Panel C was obtained with serial coughing in a woman with stress urinary incontinence, illustrating that urethral closure pressure drops to zero with coughing. Evidence suggests that pediatric overactive bladder is familial and strongly associated with overactive bladder later in life.
Syndromes
- Loss of memory
- Nephrotic syndrome
- Rash (usually small sores on the lower legs called erythema nodosum)
- Smell (normal, odorless, bad odor)
- Heart problems
- Congestive heart failure
- They work either by drawing water into the gut or by causing the muscles of the intestines to contract.
This shows four channels of radially arrayed anal pressures during a voluntary squeeze by the patient (posterior hair loss cure keratosis buy 0.5mg dutas, right hair loss in men xy discount dutas line, anterior, left). Following the quick administration and removal of a bolus of air into the rectal balloon (in this case, 20 mL), the resting pressures of the anal canal temporarily drop and then returns. It measures the speed and the magnitude of the response and provides evidence of neuromuscular health. Stimulating When performing most nerve conduction studies, a stimulus is given at a predefined site using a surface electrode. The larger, myelinated axons are depolarized first, and then the smaller, myelinated axons are depolarized. The pulse width is the duration over which the stimulus is delivered and typically ranges from 0. Recording After stimulating a nerve, a response can be measured by surface or monopolar needle electrodes. When recording a muscle response, three electrodes are necessary-an active, a reference, and a ground. The active electrode should be placed directly over the "neuromuscular junction zone" of the muscle being studied; the reference should be close, but not on the muscle, if feasible. This allows the responses recorded from the active and reference electrodes to undergo differential amplification resulting in the waveform displayed on the electrodiagnostic instrument. The ground electrode should ideally be placed between the active and reference electrodes. These recommendations are frequently not possible in pelvic floor studies, making them more challenging to perform and interpret. The response is a summation of all the muscle fibers, which are depolarized by a single stimulated nerve. Latency is affected most by the heavily myelinated or fastest conducting axons in a nerve. If the latency is long, one can assume loss of function; however, if even a few normal axons conduct the nerve impulse at a normal velocity, the latency can be normal despite significant injury. Amplitude, which is measured from baseline to the maximum point Neurophysiologic Studies Injury or trauma to the neuromuscular system as well as systemic neurologic diseases can alter anorectal function. Certain neurophysiologic tests used as an adjunct to physical examinations and other studies are used to explore the neurologic basis of certain symptoms or identify the etiology of anorectal problems. In anatomical regions outside of the pelvis, clinicians trying to determine if neuromuscular etiologies are the suspected causes of illness or disease ask the following questions: 1. Because the pelvic structures are less accessible, and the sphincter muscles are slightly different than other striated muscles in the body (smaller diameters of muscle fibers that are tonically contracting), neurophysiologic testing in the pelvis is unique. Nonetheless, the concepts of neurophysiologic testing are the same as those applied elsewhere. There are two main categories of neurophysiologic testing that can be used to sort out anorectal dysfunction: nerve conduction studies and electromyography. A of the waveform, reflects the total number of axons and muscle fibers being tested and provides an estimate of the amount of functioning tissue. Due to the potential for varying amounts of tissue between the muscle and the electrode and frequently poor impedance values, amplitude is even less reliable than latency. Duration and shape of the waveform reflect the temporal dispersion of all the individual fibers. Nerve conduction velocity is the rate at which an action potential propagates along the stimulated nerve, and is calculated by dividing the length of nerve over which the action potential travels by the time required to travel the distance. However, in motor nerve conduction studies, the latencies between two different sites of stimulation are subtracted from one another to account for the delay at the neuromuscular junction. Mark electrode is affixed to the index finger of a gloved hand in order to stimulate the pudendal nerve near the ischial spine. Close-up of the electrode demonstrating stimulating cathode and anode at the tip of the finger, with a pair of recording electrodes at the base of the finger (used for the transrectal approach). Mark electrode is attached to a gloved index finger, so the stimulating electrodes are located at the tip of the index finger and the recording electrodes at the base. Clinical Utility Pudendal nerve conduction studies are the most commonly reported electrodiagnostic tests done on the pelvic floor. Normal and Abnormal Values Normal values have been suggested by several laboratories (Table 11-2),15,17-19 each with different definitions for the normal population. Mark electrode, the latency seems to be extremely short, on the order of two milliseconds, with abnormal values in fecal incontinence defined as only a few tenths of a millisecond longer, which brings into question the clinical relevance of the test.