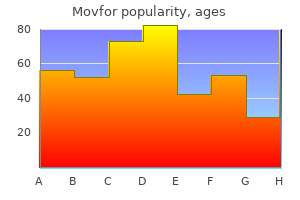
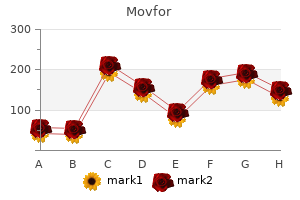
Movfor
"Generic 200mg movfor otc, hiv infection oral".
By: G. Emet, M.S., Ph.D.
Co-Director, State University of New York Downstate Medical Center College of Medicine
The final fixation of the S-hook is completed with both set screws firmly tightened hiv infection white blood cells cheap 200mg movfor amex. An L4 polyaxial pedicle screw works well to ensure proper pressure and fixation between the L4 screw and the sacral ala stages of hiv infection by who movfor 200mg with visa. Chapter 67 Anterior Approach for Open Reduction of the Developmentally Dislocated Hip Richard M. In the first trimester, the structures of the joint begin as a single mass of scleroblastema with a globular femoral head that becomes cartilage at 6 weeks. The joint space develops by degeneration at 7 to 8 weeks and the structure of the joint is well apparent by week 11. A round and reduced femoral head influences the concave shape of the acetabulum to develop. Acetabular growth depends on interstitial, appositional, periosteal new bone and secondary centers of ossification growth. In the first two trimesters of fetal life the acetabulum is a hemisphere with a depth 50% of its diameter. However, by the time of birth the depth is only 40% of its diameter, which may contribute to instability at birth. By 8 years of age the acetabular shape is for the most part determined and thus surgical reduction is less advised, especially if the dislocation is bilateral. There is continued growth into adolescence, with the triradiate cartilage fusing by 13 years in girls and 15 years in boys. The greater trochanter nucleus appears at about 3 years in girls and 5 years in boys, with the lesser trochanter appearing by age 6 to 11 years. The femoral head vascularity is mostly from the medial and somewhat from the lateral femoral circumflex arteries. Because it is an intra-articular dome-shaped structure, this blood supply is susceptible to injury. With time the neolimbus, which is abnormally formed articular cartilage, can develop at the edge of the acetabulum. Note the concentric nature of the acetabular labrum, resembling in form and function an O ring. Coronal section of a thirdtrimester fetal hip joint showing the extensive cartilaginous nature of the femoral chondroepiphysis and the acetabular cartilage. Three-dimensional computer-generated hip model of adolescent with longstanding left hip developmental dysplasia. The acetabulum is shallow and elongated in its superior aspect, resembling an egg. Clinical symptoms, typically pain, may antecede the radiographic deterioration by 10 years. If the hip is completely dislocated, limb-length discrepancy and back and knee pain are common, while painful arthritis correlates with the presence of a false acetabulum and its adverse effect on the femoral head articular cartilage. Acetabular dysplasia with no subluxation the natural history of acetabular dysplasia is much less predictable when subluxation or dislocation is absent. However, it is difficult to determine how early in life the deterioration will occur. Although hips with acetabular dysplasia can spontaneously improve, this improvement is not predictable or necessarily complete. An Ortolani-positive hip is dislocated or subluxated and the examiner perceives that the hip partially reduces with abduction. After several months of age the hip may appear stable on examination but may still be dislocated. The examiner should also note the level of the popliteal skin crease, the position of the knee, and any lateral displacement of the hip. A simple, high-pitched and commonly felt "hip click" is not a sign of instability or dislocation. Hip instability decreases with time, whereas deformity, such as limited hip abduction, increases with time. A steep, maloriented growth plate, intra-articular obstructions, and stunting of periosteal new bone formation all in time contribute to further deformity. Mechanical blocks to reduction include the anteromedial capsule, ligamentum teres, psoas tendon, neolimbus, transverse acetabular ligament (which is an inferior medial extension of the acetabular labrum), and intra-articular pulvinar tissue. Hips with acetabular dysplasia, and particularly with subluxation, have about 25% less contact area and more unit load (stress) per area of contact.
Syndromes
- Using pills to make themselves urinate (water pills or diuretics), have a bowel movement (enemas and laxatives), or decrease their appetite (diet pills)
- Females age 14 to 18 years: 1.0 mg/day
- Shortness of breath
- The stoma opening may become too small or tight. This is called stomal stenosis.
- Tremors or shaking shortly after birth
- Arterial blood gas
- Avoid touching your eyes, nose, and throat.
- Phenothiazines
- Smells
Defect reconstruction with augments and structural bone graft is required to fill the bony deficiency hiv infection prognosis buy movfor 200 mg on line. Longstemmed revision implants are required ginger antiviral cheap movfor amex, including hinged modular revision components. A custom component rarely is required because of the availability of modular oncology or limb-preserving systems. The distal femur has a 3-degree valgus slope relative to its mechanical axis and a 9-degree valgus slope relative to its anatomic axis in the coronal plane. In the sagittal plane, the proximal tibia has a posterior slope of 9 to 10 degrees on average, with a range of 4 to 12 degrees. About 60% of ground reaction forces are transmitted through the medial tibial plateau; the remaining 40% are transmitted through the lateral plateau. The trabecular bone of the proximal tibia is densest in its most proximal 1 cm and is responsible for load transmission. The strength and stiffness of the proximal tibial bone are dictated by trabecular architecture and bone density, with the most dense area being central in each plateau. The subchondral, epiphyseal, and metaphyseal bone is relatively denser in the medial tibial plateau due to higher load transmission compared to the lateral tibial plateau. The tibial tubercle is 25 to 40 mm below the joint surface, and the average insertion point of the patellar tendon is 29 mm distal to the tibial plateau. The patella tendon averages 44 mm in length and ranges from 35 to 55 mm in length. The proximal tibial periosteal blood is supplied by the medial and lateral inferior genicular arteries as well as the anterior tibial recurrent artery. The medial and lateral inferior genicular arteries arise from the popliteal artery and pass deep to the collateral ligaments to supply the medial and posterolateral periosteum of the proximal tibia. The anterior recurrent tibial artery is an ascending branch that arises from the anterior tibial artery just after it passes through the proximal tibiofibular interosseous membrane and supplies the anterolateral periosteum of the proximal tibia. All of these vessels also contribute to the anterior anastomotic peripatellar ring. The popliteal neurovascular bundle is at greatest risk during proximal tibial resection. These vessels are 3 to 12 mm posterior to the articular surface of the tibia when the leg is extended and 6 to 15 mm posterior when the knee is flexed to 90 degrees. Component subsidence, osteolysis, fracture, and infection all can alter the usual post-arthroplasty anatomy of the proximal tibia. Pre- and postoperative radiographs of the primary procedure can be invaluable during preoperative planning of the revision surgery to determine actual bone loss and true change in component position. The type of component noted on the postoperative primary radiographs can be helpful in determining the amount of bone that was originally resected from the proximal tibial plateau. Cruciate-retaining implants typically are cut with 3 to 7 degrees of posterior slope in the proximal tibial resection, whereas cruciate-sacrificing and cruciate-substituting or posterior stabilized implants typically have 0 degrees of posterior slope. Consequently, in the revision setting where posterior stabilized or "super stabilized" or "total stabilized" type components are used, additional anterior resection of the tibial plateau may be required to restore neutral slope. Some revision systems call for a slight amount of slope to match the design of the stemmed tray, and the proximal tibial should be resected accordingly. Bone defect classification schemes as outlined earlier for damaged or deficient metaphyseal tibial bone can greatly aid in understanding the pre-revision anatomy. The quantity of osteolysis is affected by implant design and the quality of polyethylene, as well as host response to particulate debris. Disuse osteopenia may contribute to massive proximal tibial bone loss in the presence of periprosthetic fracture. Component loosening and resultant implant failure occur primarily via two common routes: aseptic, due to osteolysis; and septic, due to bacterial infection. Osteolysis of the proximal tibial bone is a result of polyethylene particulate debris from wear at the bearing interface as well as "backside" wear. Somewhere on the order of billions of submicron polyethylene particles per year can be generated at the bearing surface. These particles generate histiocytic and macrophage response, where intercellular signaling pathways are activated that promote osteoclast activity and bone resorption.
There is a risk of iatrogenic injury during surgical exposure of the proximal radial shaft stages of hiv infection cdc movfor 200mg online. The ulnar nerve is tested with "scissors"-adducted thumb describe the hiv infection cycle generic 200 mg movfor otc, abducted fingers, and flexor digitorum profundus function to ring and pinky. This is the most common iatrogenic nerve injury after internal fixation of forearm shaft fractures. The median is the most commonly injured nerve after closed or open forearm shaft fractures. Flexion of the distal interphalangeal of the index finger and the interphalangeal of the thumb herald flexor digitorum profundus and flexor pollicis longus function of these digits. Isolated palsy has been reported secondary to constrictive dressings and after proximal ulna fracture. Radius Ulna Level: Fracture level has bearing on nonoperative versus operative decision making. Distal third Middle third Proximal third Pattern: Fracture pattern has bearing on nonoperative versus operative decision making. Bow (also known as plastic deformation) Greenstick Complete Comminuted respect should be paid to the level of the fractures when choosing a relatively neutral, pronated, or supinated forearm position. Price has suggested that estimated rotational malalignment should not exceed 45 degrees. An extra benefit of above-elbow immobilization relates to the activity limitation it imposes; in some instances this may increase the chances of maintaining a satisfactory reduction in an otherwise very active customer. Successful nonoperative treatment requires an eclectic mix of anatomic knowledge, skillful application of reduction techniques, appreciation for remodeling potential, and respect for the character of the soft tissue envelope. Greenstick fracture patterns retain a degree of inherent stability; intentional completion of these fractures is not recommended. Davis and Green reported a 10% loss of reduction rate with greenstick fractures and a 25% rate with complete fractures. Apex volar greenstick fractures are considered to represent supination injuries that require a relative degree of pronation to effect reduction. Apex dorsal greenstick fractures are considered to be pronation injuries that require supination to aid reduction. Classic finger-trap and traction reduction techniques are probably best reserved for complete both-bone fracture patterns. When dealing with complete both-bone shaft fractures, Flexible intramedullary nail treatment of pediatric forearm shaft fractures focuses predominantly on displaced complete fractures, many of which may have minor comminution (butterfly fragments usually less than 25% of a shaft diameter). When efforts at closed fracture management do not achieve and maintain fracture reduction within accepted guidelines, surgical treatment is indicated. Complete forearm shaft fractures in children older than 8 to 10 years of age should be evaluated very critically with the intention to accept no more than 10 degrees of angulation at any level. Preoperative Planning Rotational alignment of the radius and ulna should be assessed and estimated using the guidelines mentioned in the Anatomy section. Concern is increased if greater than 45 degrees of rotational malalignment is judged to be present. Measurement of the narrowest canal diameter of the radius (usually midshaft) and ulna (usually distal third) will aid in the selection of appropriately sized intramedullary nails. Implants 2 mm in diameter or smaller are commonly used, and the same-sized nail is used in each bone. Significant comminution may lead the surgeon to choose plate fixation over intramedullary fixation for one or both bones. Tense swelling of the forearm certainly increases suspicion for compartment syndrome, and the surgeon should be prepared to measure compartment pressures accordingly. Physeal-sparing proximal ulnar entry is typically achieved via an anconeus starting point just off the posterolateral ridge of the olecranon. The true tip of the olecranon is avoided as an entry point because it needlessly violates an apophyseal growth plate, and a subcutaneous nail in this region often leads to painful olecranon bursitis.
Diseases
- Oculocerebral syndrome with hypopigmentation
- Leukodystrophy, metachromatic
- Adrenomyodystrophy
- Stevens Johnson syndrome
- Warts
- Arginemia
- Citrullinemia