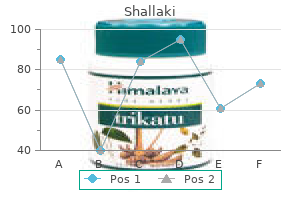
Shallaki
"Buy genuine shallaki on line, spasms vulva".
By: T. Hjalte, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Program Director, Emory University School of Medicine
The use of pharmacologic agents muscle relaxant tl 177 buy shallaki 60caps amex, specifically neuroleptics spasms the movie buy shallaki 60caps without prescription, should be reserved for patients in whom nonpharmacologic strategies do not help and the patient presents a risk of harm to self or others. The presence of comorbid illness and grief often confound the presentation of depression. As a result, it can remain undetected despite its significant adverse impact on quality of life, morbidity, and mortality. Suicide rates are almost twice as high among older persons when compared with the general population, with the rate highest for white men over 85 years of age. Among older adults, depression can present with cognitive, functional, or sleep problems, as well as complaints of fatigue or low energy. Several instruments have been developed and validated for Delirium the differential diagnosis for cognitive problems other than dementia is broad, and includes delirium, mood disturbance, and drug effects. The differentiation of dementia and delirium may present the most significant challenge, particularly in hospitalized elders (Table 126. Delirium is characterized as an abrupt change in global cognitive function, whereas dementia is chronic and affects specific cognitive domains over time. Delirium, sometimes called "altered mental status," affects more than 2 million hospitalized persons each year. Asking two simple questions about mood and anhedonia ("Over the past 2 weeks have you felt down, depressed, or hopeless When screening for depression in elders, it is particularly important to have systems in place to provide feedback of screening results, a readily accessible means of making an accurate diagnosis, and a mechanism for providing treatment and careful follow-up. Randomized trials indicate that the addition of counseling to pharmacologic therapy confers additional benefit for older, frail patients with depression. Anxiety is more common than depression among older adults and may similarly result in physical and cognitive symptoms, insomnia, agitation, psychosis, and isolation. Clinicians should consider a diagnosis of generalized anxiety, panic, or agoraphobia in older adult patients with any of these symptoms. Sleep disorders or disturbance are associated with cognitive impairment, poor health status, functional decline, and increased mortality. This may stem in part from changes in sleep structure with aging such as decreased deep (stage N3) sleep, longer sleep latency, and decreased sleep efficiency. Moreover, a variety of comorbid factors present in later life have adverse effects on sleep quality, including medical conditions, medications, psychosocial factors, and disruptive or disabling symptoms such as pain or nocturia. This includes drug and alcohol use as well as use of prescription and over-the-counter sedative hypnotics, which can cause sleep fragmentation and rebound insomnia. Additionally, medications commonly prescribed for insomnia, such as benzodiazepines and nonbenzodiazepine hypnotics, are linked with cognitive impairment and falls. The mainstay of treatment for insomnia among older adults is careful attention to addressing the variety of comorbid factors and behaviors that lead to sleep disruption. Eliciting a history of daytime somnolence and/or sleep partner complaints characteristic of these disorders should lead to completion of a diagnostic polysomnogram, which then guides initiation of appropriate therapies. Risk factors for falls include a history of falls, fear of falling, decreased vision, cognitive impairment, medications (particularly anticholinergic, psychotropic, and cardiovascular medications), peripheral neuropathy, diseases causing problems with strength and coordination, and environmental factors. Effective interventions for people with a history of falls or who are at risk for falling involve addressing multiple contributing factors. Clinicians and health care professionals should regularly inquire about recent falls or a fear of falling in older patients. For patients who report falling, the assessment should include review of circumstances of the fall(s), measure of orthostatic vital signs, visual acuity testing, cognitive evaluation, and gait and balance assessment. A time of more than 12 seconds to complete the process, or observation of postural instability or gait impairment, suggests an increased risk of falling. Gait speed, an additional measure of mobility, predicts changes in ability and health status in older adults. Gait speed is measured over a 10-meter span with the patient walking at a comfortable pace.

Onequarter of the studies that were reviewed did not report outcomes for partners spasmus nutans cheap shallaki amex. A lack of patient improvement could be explained by negative but unexamined effects on the partner or the possibility that patients and partners respond to intervention at different rates spasms cure purchase shallaki 60caps on line. Thus, future studies should include both partners and ensure that the couple is the unit of analysis throughout the research process. Another limitation is that none of the studies evaluated the costeffectiveness of couplebased interventions relative to interventions targeting the patient or caregiver alone. Understanding why some patients do not get the support they desire or expect and why certain couples are at risk for poor psychosocial outcomes will help clarify the role of couple relationships in adaptation to cancer. Researchers should recognize that relationships and relationship roles change over time. Indeed, many couples report that cancer brought them closer together, but it remains unclear what happens over time as couples learn to deal with the longterm side effects of cancer. Because the majority of couplebased studies have focused on singlegender cancers such as breast or prostate, it is difficult to disentangle gender and role. Thus, more studies should include both members of the couple and focus on cancers that affect men and women. In addition, couples at different stages of the life cycle or cancer trajectory. To date, very few studies have investigated the cancer experience of minority couples, despite the fact that a recent comparative analysis showed that cultural differences do exist-particularly around the dimensions of family boundaries, gender roles, conception of personal control, and interdependence (Kayser et al. Individuals with low socioeconomic status and those in samesex relationships have also been underrepresented in this literature. Individual factors such as attachment style and interpersonal skills may also influence relationship processes and adjustment. Few measures of cancerrelated communication exist, and those that do involve selfreports that assess the quantity rather than the quality or nature of discussions. Finally, relationship quality may be an important moderator or proxy for social support. Future intervention studies should target lifestyle behavioral changes, since partners can engage in unhealthy behaviors. Although couplebased interventions have had many positive effects, they are seldom implemented in clinical practice setting. Improved patient outcomes, such as reduced postoperative complications resulting from early identification of problems, better management of adverse effects, increased adherence to oral medication, and early detection of adverse events, would result in reduced healthcare use and costs. In addition, there is a growing need for healthcare providers to view the couple as the unit of care and provide more information and support to partners so they can provide effective caregiving for the patient while also maintaining their own health and wellbeing. Author Biographices Hoda Badr is a health psychologist and associate professor in the Department of Oncological Sciences at the Icahn School of Medicine at Mount Sinai. Her research program focuses on developing and implementing psychosocial interventions that leverage family support to improve patient and caregiver health behaviors and wellbeing across the cancer control continuum. Zeba Ahmad is an associate researcher studying psychosocial interventions with Dr. Sexual dysfunction and spousal communication in couples coping with prostate cancer. A systematic review and metaanalysis of psychosocial interventions for couples coping with cancer. Loss of lifestyle: Health behaviour and weight changes after becoming a caregiver of a family member diagnosed with ovarian cancer. Lung cancer patients and their spouses: Psychological and relationship functioning within 1 month of treatment initiation. Couples who get closer after breast cancer: Frequency and predictors in a prospective investigation. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Couples dealing with cancer: Role and gender differences regarding psychological distress and quality of life. Social support and adjustment to cancer: Reconciling descriptive, correlational, and intervention research. Enhancing dyadic coping during a time of crisis: A theorybased intervention with breast cancer patients and their partners.
Spiritual and Existential Suffering Spiritual and existential distress is prevalent in patients and families with serious illness muscle relaxant gabapentin 60caps shallaki for sale, especially at the end of life muscle relaxant wiki buy shallaki on line amex. Religion is a set of texts, practices, and beliefs about the transcendence shared by a community. The spiritual issues of seriously ill and dying patients often center on questions of meaning, value, and relationships. Dying patients want to be assured of their value in the face of actual or perceived threats to their intactness as a human being. One of the goals of palliative care is to relieve spiritual and existential distress. Examples of open-ended questions to facilitate this dialogue include: "Are you at peace with all of this Estimating and Communicating Prognosis A core component of information shared in the palliative care setting is prognosis. The range of medical and palliative options available is huge, so the challenge is to determine what makes sense to enhance the well-being of each patient at their particular stage of illness. Palliative interventions range from pure symptom management and support to invasive options, such as chemotherapy, radiotherapy, surgical/endoscopic interventions, stenting procedures, thoracentesis, paracentesis, pericardiocentesis, home inotropic therapy, noninvasive ventilation, antibiotics, or transfusions. The challenge is to individualize discussions, so that patients can take full advantage of treatments that will help them meet their goals without having their experience dominated by near futile invasive treatments. Step 3 Step 4 Step 5 Step 6 there are some patients and families that may not want to know prognosis or may want it communicated in a particular way, it is essential to begin by finding out what the patient and family knows and wants to know. Physicians tend to overestimate survival in patients with advanced cancer by about 30%, and the bias is more pronounced the longer the physician-patient relationship. Overly optimistic predictions can lead to overuse of ineffective or unwanted disease-directed treatment, delay in hospice referrals, false expectations, unnecessary tests and procedures, and poor symptom control. Therefore, accurately estimating and communicating prognosis is central to optimal decision making in advanced illness and at the end of life. In advanced illnesses, common factors found to be predictive of short-term survival. While not uniformly reliable, these criteria can be useful in formulating estimates where prognosis might be 6 months or less if the disease is allowed to run its natural course (a prognostic criterion). Therefore, it is important to integrate both evidence and experience-based medicine and present the information in formats tailored to the particular patient (verbal descriptions, numeric, frequencies, or graphics). Prognostic estimates should be bounded with ranges to convey realistic uncertainty, being sure to allow for exceptions in both directions. For example, "in my experience, patients with your condition live on average a few weeks to a few months. It could be longer, but Role of Hospice Hospice care is a specialized form of palliative care aimed at those patients and families in the terminal stages of illness. The focus of hospice relies on the belief that each of us has the right to die pain free and with dignity, and that our loved ones will receive the necessary support to allow us to do so. Since the establishment of the Medicare Hospice Benefit in 1982, use of hospice for end-of-life care has grown steadily. Cancer used to be the most common diagnosis for patients dying in hospice programs. Hospice care can also be provided in freestanding hospice centers, hospitals, and nursing homes or other long-term care facilities. Hospice criteria exist to assist in making these determinations for common medical conditions (see section, Estimating and Communicating Prognosis). The Medicare Hospice Benefit covers most costs related to terminal care without a deductible, which includes palliative medications, nursing oversight, supplies, and bereavement care. Hospice can supplement care in a skilled nursing facility, but patients themselves or their insurance would be responsible for the nursing home room and board charges. First, some may view the transition to hospice as a way of "giving up" or "giving in to death. Second, given the reimbursement restrictions, patients may also need to forgo particular types of treatment that are important to them. In order to be found to have capacity, a patient must (1) be able to comprehend the factual information about their medical condition and treatment options, (2) understand the risks and benefits of the treatment options and the consequences of that decision, (3) be able to accept or reject the proposed treatment voluntarily, and (4) provide reliable choice over time.
The Stress Concept the foundation for the scientific study of stress was firmly established by the physiologist Walter Cannon and the endocrinologist Hans Selye xanax muscle relaxant dose purchase generic shallaki canada. Woodruff as mediating key physiological changes in the body spasms during bowel movement order generic shallaki line, such as energy mobilization and increased cardiovascular function, that support the "fightorflight" response to physical threat. He proposed the theory that a wide range of experiences (stressors) have the ability to exert a similar influence on the body (stress), which can lead to detrimental effects when sustained. However, the body can detect this stress state and effectively respond by mounting a coordinated stress response. Despite the various theoretical conundrums surrounding the nature of this stress state, researchers have made a number of important discoveries concerning the neurobiology of stress. Types of Stressors the categorization of stressors into two general types, physiological and psychological, has proven useful for studying the specific underlying neurocircuitry that participates in the processing and response coordination to these stressors. Physiological stressors are those altered physiological states that elicit wellcharacterized autonomic homeostatic adjustments, such as hypothermia, hypoxia, dehydration, tissue damage, hypotension, and hemorrhage. Some of these socalled psychological (or processive) stressors are environmental stimuli that appear to be innately recognized as an immediate threat to physiological wellbeing, such as physical attack, sudden loud noise, impending collision with a fast moving object, or teetering on the edge of a high precipice. However, physiological stress responses are also effectively triggered by many other experiential situations that do not reflect impending bodily harm, such as public speaking, novel social circumstances, traffic jams, relationship difficulties, financial insecurity, and job performance concerns. Research has identified several underlying psychological factors that are shared by various psychosocial situations that are considered stressful, and these factors include lack of controllability, lack of predictability, novelty, and socialevaluative threat. The ability to respond to psychological stressors with a physiological stress response confers considerable adaptive advantage to the organism. If the organism is able to initiate a physiological stress response not only to a direct physical insult. The ability not only to respond to immediate physical stressors but also to anticipate and prepare for future stressors is a key aspect of evolutionary stress neurobiology. Types of Stress Responses Physiological and psychological stressors elicit not only a physiological response but also psychological responses. The psychological responses often include generation of emotional states, such as fear, anxiety, or frustration, as well as shifts in attention. This psychological aspect of the stress response is essential for motivation and coordination of adaptive behavioral responses. No physiological or psychological response alone, or in combination, is a dedicated response exclusively reserved for combatting stress. Each can occur in other contexts, and therefore the presence of these responses is not a definitive measure of stress, although they may be useful biomarkers associated with stress. However, because there is not a physical dimension of stressfulness inherent in stimuli, the determination of stressfulness or threat requires integrative neural processing. The perception of and the coordinated response to stress depend on hierarchically organized neural systems in the brain. In the case of an appropriate response to physiological stressors, the underlying neural circuitry tends to be relatively simple. For example, a sudden drop in blood pressure results in reduced activity of baroreceptors located in the aortic arch and carotid artery sinus. These specialized sensory neurons project via the vagus and glossopharyngeal cranial nerves to the vasomotor control centers in the brain stem. Superimposed on these evolutionarily primitive neurocircuits are more complex neural circuits and networks. The two systems mediate complementary adaptive changes in virtually every cell and system of the body, and both systems operate on a complementary time scale. Individuals do not have voluntary control over the initiation or termination of activity within these two stress response systems, but they may learn strategies, such as relaxation techniques to modulate their activity. Also depicted is an example of sympathetic postganglionic neuron projections to skin and a section of a blood vessel, where norepinephrine is released from nerve terminals. Axons of the preganglionic sympathetic neurons extend outside the spinal cord to synapse onto postganglionic cell bodies, many of which are located in sympathetic chain ganglia adjacent to the spinal column.