Dramamine
"Buy 50 mg dramamine visa, medications emt can administer".
By: H. Karmok, M.A., M.D., Ph.D.
Vice Chair, Louisiana State University School of Medicine in Shreveport
Askan G medicine 2 times a day best purchase for dramamine, et al: "Oncocytic-type" of intraductal papillary mucinous neoplasm: an analysis of 25 cases (abstract) medications gabapentin trusted 50 mg dramamine. Balci S, et al: Applicability and prognostic relevance of ampullary carcinoma histologic typing as pancreatobiliary versus intestinal, Mod Pathol 23:350a, 2010. Coban I, et al: Paraduodenal pancreatitis is one of the main causes of pseudotumor in the pancreas and periampullary region: features of a distinct entity becoming clearer, Mod Pathol 22(S1):309A, 2009.
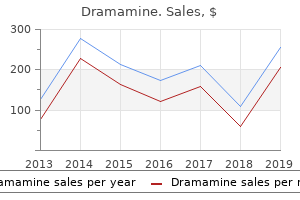
Many patients have transaminase elevations 3 to 10 times normal limits medications for rheumatoid arthritis purchase dramamine with a mastercard, indicating varying degrees of ongoing liver injury symptoms retinal detachment 50 mg dramamine overnight delivery. Most reports indicate failure of medical therapy and the need for additional intervetions. Thrombolytic therapy with urokinase or streptokinase has been used in many patients in an attempt to dissolve the thrombi and restore hepatic venous outflow (Barrault et al, 2004; Cassel & Morely, 1974; DeLeve et al, 2009; Gooneratne et al, 1979; Greenwood et al, 1983; Hodkinson et al, 1978; Hoekstra et al, 2008; Malt et al, 1978; Menon et al, 2004; Mitchell et al, 1982; Murad et al, 2009; Plessier & Valla, 2008; Powell-Jackson et al, 1982; Sharma et al, 2004; Thijs et al, 1978; Warren et al, 1972; Zimmerman et al, 2006). The experience with thrombolytic therapy has been recorded in anecdotal reports with relatively short follow-up. Approximately one-third of patients were believed to have had a clinical response to treatment for periods of 2 months to 1 year. Venogram showing stent placement (black arrows) in a recanalized right hepatic vein. The most important angiographic finding is the demonstration by hepatic venography of occlusion or marked narrowing of the major hepatic veins. In some cases, patent hepatic vein orifices cannot be identified, which is indirect evidence that all the major hepatic veins are occluded. Most often in contemporary management, venography is a platform for interventional radiology procedures. An additional advantage of hepatic venography is facilitating transjugular liver biopsy. Mild to moderate fibrosis of the liver parenchyma is found in early and subacute disease, but in chronic or rapidly progressive disease, cirrhosis of the cardiac type develops. However, thrombolytic therapy combined with angioplasty has produced more durable results in select contemporary reports. In a recent series from China, 12 or 13 patients had patent hepatic veins without recurrent thrombosis after a mean follow-up of 24 months. The one initial treatment failure was salvaged by repeat angioplasty (Zhang et al, 2013). Administration is best accomplished with catheter-directed methods, although systemic delivery has been described for other indications. Careful monitoring is required for systemic delivery in particular because of a high risk of bleeding. Single case reports have described successful thrombus resolution with systemic thrombolysis alone (Clark et al, 2012). Most reports of the effectiveness of this form of treatment have been anecdotal and lack long-term follow-up. There is no evidence that the use of either heparin or warfarin (Coumadin) brings about dissolution of established thrombosis. Newer oral anticoagulants, such as the factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban) and the direct thrombin inhibitors. In all cases, the pressure gradient that existed before balloon dilation was substantially reduced or eliminated at the time of dilation. Most of the patients have not had long-term follow-up, so it is difficult to evaluate the ultimate effectiveness of percutaneous transluminal angioplasty. Mancuso and associates (2003) described a series of 15 patients, with five deaths and one technical failure, a 40% negative outcome. Perello and colleagues (2002) reported a series of 13 patients with three shunt failures (23%). Most of the reports have involved retrospective reviews of small numbers of cases followed for short periods. The mortality rate without and with the patients lost to follow-up was 20% and 30%, respectively. Primary patency has dramatically improved with the advent of covered stents and is better than 75% in larger series, with secondary patency of 99% at a mean follow-up of 82 months (Tripathi et al, 2014). In this single-center experience, long-term follow-up included 72% survival at 10 years. The largest reported systematic review looked at 2255 patients treated with percutaneous techniques (Zhang et al, 2015). Overall survival for any interventional strategy was 92% at 1 year and 76% at 5 years.
Heterotopic pancreas was the indication for surgery in 36% of cases medicine the 1975 buy generic dramamine from india, and in 45% medicine qvar inhaler order dramamine 50 mg line, it was diagnosed incidentally during surgery. In 18% it was diagnosed on gastroduodenoscopy, and definitive surgical management was not required. In the majority of cases found at open surgery, the lesion was resected even when thought to be asymptomatic. This is advised because the diagnosis cannot be made clinically, and the main differential is malignancy. A frozen histologic section is an alternative approach but is rarely worthwhile unless an extensive resection is required. When identified at endoscopy, initial biopsies are often negative because the overlying mucosa may be normal. If the lesion is thought to be symptomatic, a resection can be planned, but many can be treated conservatively with no negative long-term consequences. Aoki T, et al: Is preventive resection of the extrahepatic bile duct necessary in cases of pancreaticobiliary maljunction without dilatation of the bile duct Cameron G: Pancreatic anomalies: their morphology, pathology and clinical history, Trans Coll Phys 46:781, 1924.
Late in the course treatment ear infection order dramamine 50 mg without prescription, the damage to the hepatic parenchyma becomes irreversible; thus the timing of therapy has profound implications for the prognosis useless id symptoms order dramamine 50 mg free shipping. These veins ultimately form the basis for intrahepatic shunts because they are the only site for adequate parenchymal drainage. The thrombus undergoes organization and ultimately is converted to fibrous tissue that permanently occludes the veins. Although recanalization of the occluded veins sometimes occurs, it rarely results in effective new outflow channels. Indeed, chronic congestion of the liver leads to some degree of irreversible parenchymal injury. Retrograde propagation of the thrombus into smaller hepatic veins is typically found. Most of the cases have run a chronic course before discovery, and when first seen by a physician, patients have extensive hepatic fibrosis or cirrhosis with portal hypertension and all its manifestations. Patients can have an acute or subacute course (typical for patients in Western countries), with rapid progression of liver disease and its consequences during a few weeks to a few months. B-mode (A) and color Doppler (B) ultrasound images showing patent transjugular intrahepatic portosystemic shunt (arrows) with appropriate flow direction and velocity. However, in another contemporary single-center experience, most patients presented with advanced disease at diagnosis, with 92% exhibiting ascites and 55% with cirrhosis (Pavri et al, 2014). In his collected series of 133 patients, Parker (1959) observed that 57% had symptoms for 3 months or less, and 71% had been symptomatic for 6 months or less. The reported incidence of ascites ranges from 83% to 100% in the larger reported series (Mitchell et al, 1982; Orloff et al, 2012; Parker, 1959; Pavri et al, 2014). Hepatomegaly resulting from severe congestion of the liver occurs in most patients. Substantial wasting as a result of loss of lean body mass during a relatively short time is observed in many patients. Signs of portal hypertension are often exhibited, including distension of abdominal veins and palpable splenomegaly. The initial symptom in the majority of patients is abdominal distension secondary to ascites, which increases progressively over a few weeks. The spectrum of pain is localized to the right hypochondrium, diffuse in the upper abdomen, or diffuse throughout the abdomen. The underlying pathophysiology is likey distension of the liver capsule from intense hepatic congestion or rapid accumulation of ascites. Additionally, these patients are often malnourished, may exhibit severe anorexia, and can exhibit mild jaundice. Early in the acute setting, Budd-Chiari syndrome is demonstrated on sagittal (A) and coronal (B) computed tomographic images, with subtle thrombosis in the hepatic veins with nonopacification (black arrow) and a smooth liver contour. With time, prominent intrahepatic vessels can be seen (C), ascites develops, significant caudate hypertrophy occurs (D, white arrow), and heterogeneous enhancement is seen with central hyper- and peripheral hypo-enhancement (E). Regenerative nodules often form, with arterial enhancement persisting through the venous phases, in contrast to hepatocellular carcinoma, which typically demonstrates washout in the venous phase. Further sequelae seen on axial magnetic resonance images include development of diffuse nodular disease (A); growth of large intrahepatic, often comma-shaped collaterals (B, white arrow); and intrahepatic shunts (C, black arrow) between the portal system and the caudate lobe. Venogram of the inferior vena cava demonstrates compression of the intrahepatic portion of the cava (A, black arrows) during placement of a transjugular intrahepatic portosystemic shunt (single black arrow). Most often, one of the occluded veins can be cannulated, often showing thrombus (B, black arrow). Further injection after accessing the hepatic vein may demonstrate the classic "spiderweb" pattern of small, intrahepatic venous collaterals (C). This study may occasionally be combined with hepatic and superior mesenteric arteriography and indirect portography. This finding usually is not clinically significant unless severe compression precludes surgical shunting. Both these cardiac disorders can be eliminated easily from consideration by appropriate cardiac functional studies. A wedge liver biopsy specimen obtained at operation showed intense centrilobular congestion and marked centrilobular cell loss and necrosis in all but one patient, and 35 (54%) of the 65 patients had hepatic fibrosis; this was mild or moderate in 30 patients and severe in five patients, four of whom had cirrhosis. These procedures are crucial options for some patients, however, and require the skill and experience typically seen only in specialized centers. In the mesoatrial shunt, a midline laparotomy combined with a median sternotomy is the standard approach.