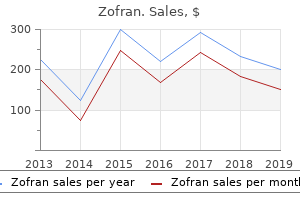
Zofran
"Purchase generic zofran online, medications used to treat fibromyalgia".
By: A. Faesul, M.B. B.A.O., M.B.B.Ch., Ph.D.
Assistant Professor, The University of Arizona College of Medicine Phoenix
Table 4: Pelvic dimensions in female pelvis Diameter Anteroposterior Oblique Transverse At inlet 11 12 13 At mid-pelvis 12 12 12 At outlet 13 12 11 851 Self Assessment and Review of Anatomy Diagonal conjugate is the distance from the sacral promontory to the inferior margin of the pubic symphysis symptoms intestinal blockage order zofran 8mg on-line. Obstetric conjugate is the least (shortest) anteroposterior diameter of the pelvic inlet from the sacral promontory to a point a few millimeters below the superior margin of the pubic symphysis (>10 cm) medications that interact with grapefruit discount zofran on line. True conjugate is the distance from the sacral promontory to the superior margin of the pubic symphysis. The ischial spines may present a barrier to the fetus during childbirth if the interspinous diameter is less than 9. Sacroiliac Joint is a plane synovial joint between the auricular surfaces of the sacrum and ilium. It is covered by cartilage and is supported by the anterior, posterior, and interosseous sacroiliac ligaments. Sacrococcygeal Joint is a symphysis (secondary cartilaginous) joint between the sacrum and coccyx, reinforced by the anterior, posterior, and lateral sacrococcygeal ligaments. Pubic Symphysis is also a fibrocartilaginous joint between the two hip bones, joined anteriorly by a fibrous cartilage covered by a hyaline cartilage in the median plane. Nerve Supply Nerve supply to pelvic viscera (like urinary bladder, uterus, rectum etc. Neurone bodies of vagus nerve are present in the dorsal nucleus of vagus (medulla oblongata) Preganglionic neuronal cell bodies are located in the gray matter (intermedio-lateral horn cells) of the S2 to S4 spinal cord and form the pelvic splanchnic nerves. Postganglionic neuronal cell bodies are located near or within the respective viscera. It is the downward continuation of the aortic plexus (intermesenteric plexus) from the inferior mesenteric ganglion. Beginning below the aortic bifurcation and extending downward retroperitoneally, this plexus is formed by sympathetic fibers arising from spinal levels (T10-12; L1-2). It descends anterior to the L5 vertebra and at the level of the sacral promontory, this superior hypogastric plexus divides into a right and a left hypogastric nerve, which run downward along the pelvis side walls and lies in the extraperitoneal connective tissue lateral to the rectum. Hypogastric nerves provides branches to the sigmoid colon and the descending colon and is joined by the pelvic splanchnic nerves to form the inferior hypogastric (or pelvic plexus). Superior hypogastric plexus contains preganglionic and postganglionic sympathetic fibers, visceral afferent fibers, and few, if any, parasympathetic fibers, which may run a recurrent course through the inferior hypogastric plexus. Inferior Hypogastric Plexus (also termed the pelvic plexus) is formed by the union of two hypogastric nerves (sympathetic), two pelvic splanchnic nerves (parasympathetic), and sacral splanchnic nerves (L5 and S1 to S3). It is retroperitoneal collection of nerves lying at the S4 and S5 level, against the posterolateral pelvic wall, lateral to the rectum, vagina, and base of the bladder. It contains pelvic ganglia, in which both sympathetic and parasympathetic preganglionic fibers synapse. Fibers of this plexus accompany internal iliac artery branches to their respective pelvic viscera. It gives rise to rectal plexus, utero-vaginal plexus, vesical plexus, and prostatic plexus. Vesical plexus innervates the bladder and the middle rectal travels to the rectum. Uterovaginal plexus (Frankenhauser plexus), reaches the proximal fallopian tubes, uterus, and upper vagina. Extensions of the inferior hypogastric plexus also reach the perineum along the vagina and urethra to innervate the clitoris and vestibular bulbs. Sacral Splanchnic Nerves consist of preganglionic sympathetic fibers that come off the sympathetic chain and synapse in the inferior hypogastric (pelvic) plexus.
This trend held significance when comparing fixation methods among patients with inflammatory diagnoses only symptoms before period discount 4mg zofran amex. However treatment zinc toxicity buy cheap zofran 8 mg on-line, the clinical importance of breakage where an osseous fusion has been obtained is not clear. If there is no subsidence, placement of a lumbar drain may be indicated, followed by possible surgical wound revision. With regard to occipitocervical fixation, the amount of metallic material and the distribution defined by the moment area of inertia, or resistance to angular acceleration, has a large effect on the biomechanical performance because of its direct correlation with stiffness. Screws are ideally placed in areas with thick bone because pullout strength is dependent on bone thickness and number of cortices engaged. In general, bone is thickest in the midline at the external occipital protuberance and is largely dense, cortical bone ranging from 11 to 17. Furthermore, because bone thickness decreases radially from the protuberance, screw pullout strength is greatest above the superior nuchal line. That is, although midline screws may have greater pullout strength because the anatomy accommodates longer screws, lateral screws provide increased stiffness in rotation and bending but not flexion and extension. Earliest implants consisted mostly of posterior wiring techniques often requiring extension to caudal levels to ensure stability, as well as supplemental external stabilization, often in the form of halo vests, because of insufficient initial stabilization. Today, the most popular configuration is composed of various cervical screw configurations along with an occipital plate fixed with occipital screws connected by a contoured rod. Thus, the surgeon must be familiar with the various implants so that stability is optimized while osseous fusion is obtained. Winegar et al1 investigated the cause of failure of all reported occipitocervical arthrodeses constructs in the literature from 1969 to 2010. They reported a 21% instrumentation failure rate overall with wiring being the most likely to fail (10. Complications of Occipital Instrumentation With regard to occipital screw choice, no biomechanical advantage has been demonstrated between cancellous and cortical screws. That is, most current occipital screws are unique in that they have a larger diameter and smaller pitch, which allows for greater contact area in areas of thin bone. Its safety and biomechanical effectiveness have both been shown in multiple studies. Occipital plates that include a suboccipital extension for direct connection to the cervical spine, such as Y plates, are particularly problematic in this respect. Furthermore, appropriate screw positioning often poses a real surgical challenge because of its limited positioning options. Most modern constructs composed of an independent occipital plate connected by bars to cervical screws permit anatomic contouring and allow for more facile screw placement and less prominence. Most occipital plates offer sagittal and coronal pre-bend regions for contouring in both planes. Other rod types do exist and include rods that transition to an occipital plate cephalad. Regardless of the implant chosen, fastidious attention to instrumentation contouring to avoid prominence should be employed. The design that affords the surgeon the greatest modification is modular implants, or those with an independent rod attached to occipital plates by dedicated anchors. This connection also varies; some offer multidirectional tuning and others are fixed angle in nature. Independent occipital plates allow the greatest flexibility for hardware placement and individual intraoperative component modification without necessitating entire construct removal. An adjustable rod with a manufactured joint may also be selected, which allows for adjustment in one plane and precludes the need for bending, which may result in less fatigue failure. This is especially important to consider when using titanium rods, as these are notch sensitive in fatigue failure, so that longer curves should be implemented at the craniocervical junction rather than acute bends as is often required.
The thoracic nerves enter the rectus sheath at its lateral margin and pass posterior to rectus abdominis symptoms inner ear infection zofran 8 mg on-line, where they again intercommunicate symptoms 0f colon cancer cheap 4mg zofran. Each nerve then pierces rectus abdominis from its posterior aspect and gives off muscular branches to this muscle (and a branch to pyramidalis from the subcostal nerve), and cutaneous branches that pierce the anterior rectus sheath to supply overlying skin. The ninth intercostal nerve supplies skin above the umbilicus, the tenth supplies skin that consistently includes the umbilicus, and the eleventh supplies skin below the umbilicus. The subcostal nerve supplies the anterior gluteal skin just below the iliac crest, and the skin of the lower abdomen and inguinal region (overlapping with the L1 dermatome in this region) the ventral rami of the lower intercostal and subcostal nerves also provide sensory fibres to the costal parts of the diaphragm and parietal peritoneum. Using ultrasound imaging guidance, local anaesthetic is injected into the neurovascular plane between internal oblique and transversus abdominis, targeting the segmental nerves of the anterolateral abdominal wall. Lesions of the Intercostal Nerves the anterolateral abdominal wall muscles are innervated by several segmental nerves and injury to a single nerve does not 736 the overlap between sequential dermatomes means that significant cutaneous anaesthesia is appreciated only after sectioning at least two sequential nerves. It does not enter the rectus sheath and its lateral cutaneous branch supplies the skin of the gluteal region. It pierces the internal oblique muscle from below and enters the inguinal canal lateral to the iliohypogastric nerve, and It comes out through the superficial inguinal ring. It arises at the level of the sixth costal cartilage and descends between the costal and xiphoid slips of the diaphragm, the vessels pass anterior to the lower fibres of transversus thoracis and the upper fibres of transversus abdominis before They anastomose with the inferior epigastric arteries, usually above the level of the umbilicus, in one of several potential Branches supply rectus abdominis and perforate the anterior lamina of the rectus sheath to supply the abdominal skin. A branch given off in the upper rectus sheath passes anterior to the xiphoid process of the sternum and anastomoses with this vessel may give rise to bleeding during surgical incisions that extend up to and alongside the xiphoid process. The superior epigastric artery also gives small branches to the anterior part of the diaphragm. On the right, small branches reach the falciform ligament, where they anastomose with branches from the hepatic artery. Inferior Epigastric Artery and Veins the inferior epigastric artery (Often referred to as the deep inferior epigastric artery in clinical practice in order to distinguish 738 accompanied by two or more veins that drain to the internal thoracic vein. Its accompanying veins, usually two, unite to form a single vein that drains into the external iliac vein. It curves forwards in the anterior extraperitoneal tissue and ascends obliquely along the medial margin of the deep inguinal ring. It lies posterior to the spermatic cord, separated from it by the transversalis fascia. It pierces the transversalis fascia and enters the rectus sheath by passing anterior to the arcuate line. In this part of its course, it is visible through the parietal peritoneum of the anterior abdominal wall and forms the lateral umbilical fold. The inferior epigastric arteries ascend and anastomose with their superior counterpart without branching in about 30% of cases. Branching into two vessels before anastomosis is the most common pattern, accounting for almost 60% of cases, with a trifurcation being present in the remainder. The inferior epigastric arteries have an average diameter of approximately 3 mm at their origin, compared to an average diameter of 1. Preliminary ligation of the inferior epigastric artery is often performed when preparing a myocutaneous flap using the mid or lower rectus abdominis based on the superior epigastric artery; this encourages the augmentation of the superior epigastric arterial supply. Branches of the inferior epigastric artery anastomose with branches of the superior epigastric artery within the rectus sheath posterior to rectus abdominis at a variable level above the umbilicus. Other branches anastomose with terminal branches of the lower five posterior intercostal, subcostal and lumbar arteries at the lateral border of the rectus sheath. The inferior epigastric artery ascends along the medial margin of the deep inguinal ring. The vas deferens in the male, or the round ligament in the female, passes medially after hooking around the artery at the deep inguinal ring. The inferior epigastric artery also gives off the cremasteric artery, a pubic branch, and muscular and cutaneous branches. The cremasteric artery accompanies the spermatic cord in males, supplies cremaster and the other coverings of the cord and anastomoses with the testicular artery. A pubic branch, near the femoral ring, descends posterior to the pubis and anastomoses with the pubic branch of the obturator artery.
Syndromes
- Post-traumatic stress disorder
- A balloon, which is placed under your belly muscles. It holds the same liquid as the cuff.
- Skin infection (cellulitis)
- Hyperthyroidism (overactive thyroid)
- Discomfort
- Acute pyelonephritis
- Shock
- Occur during sleep
- Magnetic resonance arteriography (MRA) is a special type of MRI scan
If injured medicine to increase appetite generic 8mg zofran with amex, it leads to an ipsilateral curvature of the tongue and slurring of speech medicine xyzal cheap zofran 8 mg free shipping. Many of the potential complications with these techniques are related to the surgical approach and the infrequency of the surgical anatomy in the anterior cervical spine for many spine surgeons. Both the anterior and lateral retropharyngeal approaches each encounter several neurovascular structures that must the identified and preserved. Diluted methylene blue is then placed down the tube (~ 60 m) and the wound checked for egressing blue fluid. If no evidence of perforation is seen but still strongly suspected, intraoperative esophagoscopy by otolaryngologist is warranted, given the high morbidity and mortality if left untreated. Once identified, the defect is closed in two layers and the nasogastric tube left in place for 7 to 10 days, along with parenteral antibiotics against anaerobic bacteria administered. For transarticular screw placement, axial imaging must to meticulously reviewed for any medialization of the artery at C2, which would prevent such a technique. For plate placement, the lateral C1 screws should be placed in a near direct anterior to posterior direction on the axial plane and not directed superiorly in the sagittal plane to minimize the risk of vertebral artery injury. Given the high-density nature of the upper cervical spine, both hold potential risks to vital nerves by transection and/or excessive traction. The surgeon should remain aware throughout the approach to include the greater auricular nerve, marginal mandibular branch of the facial nerve, superior laryngeal nerve, spinal accessory nerve, and hypoglossal nerves. No matter if transarticular screws are placed using an antegrade or retrograde technique, particular attention should be Kim et al. Anterior C1-C2 screw fixation and bony fusion through an anterior retropharyngeal approach. Atlantoaxial fusion using anterior transarticular screw fixation of C1-C2: technical innovation and biomechanical study. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Comparison of the anatomic risk for vertebral artery injury associated with percutaneous atlantoaxial anterior and posterior transarticular screws. Complications of Odontoid Fracture Treatment 14 Complications of Odontoid Fracture Treatment Steven Presciutti, Brian Tinsley, and Isaac Moss 14. Fracture of the odontoid process can be highly unstable and may result in significant neurologic injury due to its proximity to the brainstem and spinal cord. These are generally not amenable to reduction and fixation with an anterior screw and necessitate posterior fixation. Treatment is guided by the type of odontoid fracture and the specific fracture orientation. By definition, however, the avulsion fracture that makes up a type I indicates that at least one of the two alar ligaments is incompetent. The alar ligaments are important in maintaining craniocervical stability, and thus these type I injuries may be associated with occipitoatlantal instability. Regardless of how type I fractures are treated, however, it has been shown that there is a very low rate of nonunion. Historically, these injuries have been treated with a variety of surgical and nonsurgical approaches. In the modern era, however, much of the recent analysis has demonstrated acceptable healing with nonoperative treatment. While not common, there are many proponents for the use of nonrigid immobilization.